My Dentist’s Misdiagnosis Led to Unnecessary Tooth Extraction
 I was sensitive to cold foods and drinks in my lower right first molar, and my toothache felt worse if I touched the tooth. Since I didn’t have a regular dentist, I used an advertising dentist I had seen on TV and billboards.
I was sensitive to cold foods and drinks in my lower right first molar, and my toothache felt worse if I touched the tooth. Since I didn’t have a regular dentist, I used an advertising dentist I had seen on TV and billboards.
The dentist said I had three impacted wisdom teeth, and one may be pushing on a nerve. He also recommended a filling in my tooth. After the filling, my tooth pain increased, so the dentist adjusted my bite and prescribed antibiotics. He told me to take over-the-counter pain medications. The tooth didn’t improve, so the dentist referred me to an oral surgeon for wisdom tooth removal. The first molar tooth still hurts, and I explained that the pain is not near my wisdom teeth.
Two days later, I went to the ER, and they took an X-ray, explaining that I had an abscess. My dentist referred me to an endodontist who was booked for three weeks. The oral surgeon agreed that I had an abscess but recommended an extraction since I couldn’t get a root canal. Now, I have lost a tooth and am out of hundreds of dollars for this nonsense. How can I get my money back? – Thank you. Ryan
Ryan,
Your dentist made severe mistakes in diagnosing and treating your oral pain. We recommend demanding that the dentist pay for your oral surgeon and ER visits and the cost of a dental implant to replace your missing first molar. Explain that you are willing to file a malpractice claim for damages.
Dental Diagnostic and Treatment Mistakes
The mistakes your dentist made with your first molar toothache include the following:
- Failure to recommend root canal treatment – Your toothache, increased pain when touched, and temperature sensitivity indicated that you needed root canal treatment. Bacteria caused tooth inflammation and probably spread to the root tip, which would cause sensitivity.
- Unnecessary dental filling and antibiotics —Your dentist placed a filling for deep decay and adjusted your bite. Also, the antibiotic prescriptions suggest that he may have thought you had a tooth infection yet did not recommend root canal treatment or refer you to an endodontist. Still, antibiotics alone do not remedy a tooth infection—root canal treatment does.
- Facial swelling—After seeing your swelling, it should have been clear that you had an infection. However, you had to go to the ER for help. Your dentist still didn’t drill an opening in your tooth to relieve your pain, which would have helped.
- Referral to an endodontist who couldn’t help promptly – Finally, after getting a referral, the endodontist couldn’t see you for two weeks. Your dentist should have done everything possible to find a specialist for prompt treatment.
What Can You Do If Your Dentist’s Treatment Was Unnecessary?
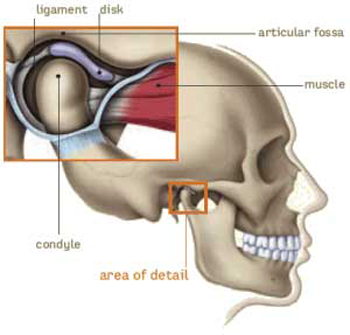
If your dentist’s treatment was unnecessary, you may allow them to pay for it before filing a legal claim. Your dentist should be willing to pay to replace your mistakenly extracted tooth with a dental implant. If your dentist is uncooperative, you may seek an attorney. Replacing the tooth is vital to prevent other teeth from drifting. Otherwise, the issue may disrupt your bite and lead to TMJ disorder.
Dr. Thaddeus Michalski, a Rocky Hill, Connecticut dentist and Diplomate of the International Congress of Oral Implantologists, sponsors this post.
What Can I Do If a Root Canal Filling Fell Out?
I had a root canal in March 2023. Within six months, I lost my job and dental insurance. I had not been to a dentist since that time. I now have dental insurance, so last week, I went for an exam and to get a consultation for teeth whitening. The dentist told me that the temporary cap is coming off the tooth, and the root canal filling is coming out. The metal post in my tooth is showing. I need to get it replaced before I get my teeth whitened. I was not planning on this type of expense right away. I am still catching up on bills. I just wanted to make my smile look good and feel a little better about myself. Is this something that must be fixed now, or can I find someone else to do the whitening? Thanks. Tracie
Tracie,
You need a dentist to replace the filling material. We understand that your financial situation has not improved enough for major dental work, but if the dentist you saw is not willing to do it inexpensively, you can find one who will do it.
Root Canal Filling Material
Root canal filling material replaces the tooth pulp that a dentist cleans out of an infected tooth. But the filling material must be protected to prevent saliva and fluid from leaking in and reinfecting the tooth. A reinfected tooth needs repeat root canal treatment to save it.
Protecting the filling material – After root canal treatment, a dentist can protect the filling material in several ways:
- Insert a metal post in the tooth and fill the tooth with a bonding material.
- Place a temporary crown over the tooth
- Place a permanent crown over the tooth
Although a filling over the tooth can last several years, eventually, you will need a dental crown.
When Root Canal Filling Comes Off
When root canal filling comes off, you must have a dentist replace it right away. It is the only way to save the tooth and prevent repeat root canal treatment.
Your oral health is the priority – Although we understand that you want to improve your smile with teeth whitening, any conscientious dentist will recommend stabilizing your oral health first. Bleaching treatment can irritate unhealthy teeth. A bright smile with a tooth that is in jeopardy of falling out is not a healthy smile. Please make oral health your priority and get teeth whitening afterward.
Rocky Hill, CT, dentist Dr. Thaddeus Michalski sponsors this post.
How Much Dental Work Can I Get In One Visit?
Hi. I really don’t like going to the dentist. I want to finish dental work without too many dental appointments. I need two crowns and three root canals, and I want to get my teeth whitened. I put off the root canals and crowns for over a year. My dentist wants me to spread the treatment over two months, but I would like this done all at once. I don’t like a dentist who has me return unnecessarily. Can I get all this work done on the same day, or am I not being reasonable? – Ken from Reno, NV
Ken – Thank you for your question. We understand your concerns about minimizing dental visits and maximizing your time in the dental chair.
How Much Dental Work Can You Get in One Visit?
How much dental work you can get in one visit depends on several factors, including:
- The type of procedure
- Procedure complexity
- Extent of the work required
- Condition of your teeth
- Your oral health
- Your physical health
- Your dentist’s experience, skills, and recommendations
- Whether you get dental sedation and the type of sedation
How Does Sedation Dentistry Help a Dentist Accomplish More?
 Sedation can help a dentist accomplish more work than without sedation for these reasons:
Sedation can help a dentist accomplish more work than without sedation for these reasons:
- You are relaxed – A patient’s anxiety, gag reflex, or inability to relax can limit how much work a dentist completes in one visit. However, dental sedation calms you and allows a dentist to proceed with treatment.
- Your dentist can focus – Your relaxed state allows the dentist to focus on your care while monitoring your vital signs during sedation.
- Decrease pain sensitivity – The American Dental Association confirms that using sedation for complex treatments can ease pain and anxiety.
Can You Get Teeth Whitening and Crowns on the Same Day?
A dentist must complete teeth whitening before placing dental crowns. Your dentist will want to ensure the crowns match your whitened teeth. It can take a week or two for your tooth color to stabilize after whitening.
Speak with your dentist regarding your concerns about minimizing your visits and making your visits as productive as possible. Ask your dentist about sedation for your procedures, too. Consider getting a second opinion from an advanced cosmetic dentist if necessary.
Dr. Thaddeus Michalski, a Rocky Hill, Connecticut dentist and Diplomate of the International Congress of Oral Implantologists, sponsors this post.
Why Does My Root Canal Tooth Hurt After Weeks of Antibiotics?
My second molar root canal tooth still hurts, although my dentist completed the root canal in August of this year. My dentist prescribed antibiotics twice, but the tooth still hurts. The pain is severe when I chew. Should I ask her for more antibiotics, or is something else wrong? Thank you. Anita from Dover, DE
Anita,
Thank you for choosing our office for your question.
Although Dr. Michalski would need to examine your tooth and x-rays for an accurate diagnosis, we can explain what may be happening.
What Causes Continued Pain After Root Canal Therapy?
Causes of pain after root canal therapy may include these factors:
- Untreated root canals – Sometimes, a tooth has multiple or curved channels. The condition will persist if your dentist misses canals or cannot clear the infection from curved canals.
- Infection in another tooth – Pain from another infected tooth can refer to the root canal tooth.
- Irritation and inflammation – Clearing infection from a tooth can irritate it, leaving it inflamed and sensitive. It can take several weeks for the sensitivity to fade. A dentist may make a thin custom mouth guard to wear and night and relieve the pressure on the inflamed tooth. Otherwise, continued stress on the tooth can lead to jaw pain, earaches, headaches, and other TMJ symptoms.
- Irritation from crown preparation– Removing tooth structure to prepare the tooth for a dental crown can irritate it. The irritation should improve gradually.
Questions to Ask to Determine the Source of Discomfort
An accurate diagnosis includes asking you these questions:
- Is your discomfort better, worse, or the same after root canal therapy?
- Do you feel sensitivity to heat or cold in the tooth?
- Other than chewing, what triggers the pain?
Ask your dentist for an x-ray to ensure she cleaned the infection from all the canals. If canals are challenging to detect or reach, your dentist must refer you to an endodontist (root canal specialist) for further treatment. Specialists have tools designed to reach challenging canals.
Rocky Hill, Connecticut dentist Dr. Thaddeus Michalski, sponsors this post.
Can a Dentist Save My Tooth Without a Post and Core?
I expected my dentist to tell me I needed a root canal, but he also mentioned adding a post and core. I did not fully understand her explanation about why I needed the post and score. It seemed that she was repeating something she had read in a textbook. I am anxious about a root canal, but a post and core sound like a long appointment. When are a post and care necessary? Thank you. Noah from Detroit, MI
Noah,
Thank you for your question. Dr. Michalski would need to examine and x-ray your tooth for an accurate diagnosis, but we will explain the purpose of a post and core, when it is required, and how it affects the long-term outcome of a tooth.
What Are a Dental Post and Core?
A dental post and core are materials to strengthen a tooth weakened by decay, damage, and root canal treatment. The post is a small cylinder that supports a core. The core is a dental filling material that replaces the tooth pulp and supports a dental crown.
Why Would a Dentist Recommend a Post and Core?
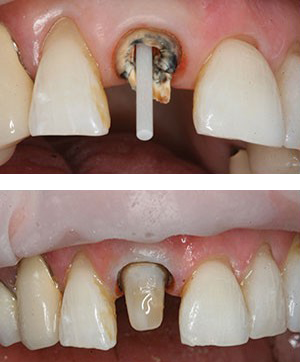
A dentist may recommend a post and core so that your tooth can support a dental crown. Sometimes, preparing your tooth for a crown requires a dentist to remove a lot of decay or damage, leaving a small amount of tooth structure. The core, or dental filling material, will replace the tooth structure and allow a dentist to cement a crown on the tooth.
The process includes these steps:
- Complete root canal therapy to remove tooth decay and infection
- Place one or two posts into the tooth
- Fill the tooth with dental material
- Build up and shape the tooth with dental bonding
- Bond a dental crown to the tooth
Will You Lose Your Tooth Without a Post and Core?
Declining a post and core may result in tooth loss for these reasons:
- You may not have enough tooth structure to support a dental crown.
- Your tooth can become weak and brittle.
- Without a post and core, you may need an extraction and dental implant
Please keep in mind that if you lose the tooth, replacing it with a dental implant and crown can cost $3,000 to $5,000 depending on these factors:
- Condition of surrounding gums and bones
- Procedures you may need in preparation for an implant
- Dental fees in your location in the U.S.
If you are unsure about your dentist’s recommendation for a post and core, schedule a second opinion with an advanced cosmetic dentist trained in root canal therapy and dental implants.
Dr. Thaddeus Michalski, a Rocky Hill, Connecticut dentist and Diplomate of the International Congress of Oral Implantologist, sponsors this post.
Root for Root Canal Therapy in Rocky Hill, CT
 If you had a bad toothache, would you rather save the tooth or have the tooth pulled? The answer, of course, is practically obvious. Save the tooth! More often than not, saving a tooth may require a root canal, especially if the toothache is caused by an infection deep within the tooth. With root canal therapy, Dr. Thaddeus S. Michalski and his staff in Rocky Hill, CT, can save the tooth and your smile.
If you had a bad toothache, would you rather save the tooth or have the tooth pulled? The answer, of course, is practically obvious. Save the tooth! More often than not, saving a tooth may require a root canal, especially if the toothache is caused by an infection deep within the tooth. With root canal therapy, Dr. Thaddeus S. Michalski and his staff in Rocky Hill, CT, can save the tooth and your smile.
A root canal is dental procedure that removes infected pulp tissue from the innermost part of a tooth. Dental pulp is comprised of nerve and lymph tissue, as well as blood vessels. This pulp may become infected as a result of oral bacteria that migrates to the pulp through a deep cavity; a crack in the tooth that penetrates the pulp; or a powerful hit to the face. The resultant infection can cause significant pain and runs the risk of spreading beyond the tooth.
The signs and symptoms of diseased or infected tooth pulp may include:
- Moderate to severe tooth pain
- Swollen gums around the affected tooth
- A tooth that is discolored
- Visible signs of infection on an x-ray
Once Dr. Michalski confirms that a tooth is deeply infected, he will recommend root canal therapy. During a root canal, Dr. Michalski will clean out the bacteria and infection, as well as remove the nerve, lymph and blood tissue from inside the tooth and its roots. The tooth is filled with a material that prevents the infection from returning, and then the tooth is typically outfitted for a protective crown that ensures the tooth’s strength and functionality. Once the root canal is completed and the crown is in place, the tooth can last for a lifetime with proper brushing, flossing and regular dental check-ups.
Call the Office of Dr. Michalski Today
If you are experiencing tooth pain, don’t delay for another moment. Call the office of Dr. Michalski in Rocky Hill, CT, where he and his staff will gently and professionally determine the cause of your pain and whether or not a root canal is the solution. Our office also serves patients in Hartford, Wethersfield, Cromwell, Newington and Berlin.


